
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Exercise, Mitohormesis, and Mitochondrial ORF of the 12S rRNA Type-C (MOTS-c)
- Tae Kwan Yoon, Chan Hee Lee, Obin Kwon, Min-Seon Kim
- Diabetes Metab J. 2022;46(3):402-413. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0092
- 5,358 View
- 238 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
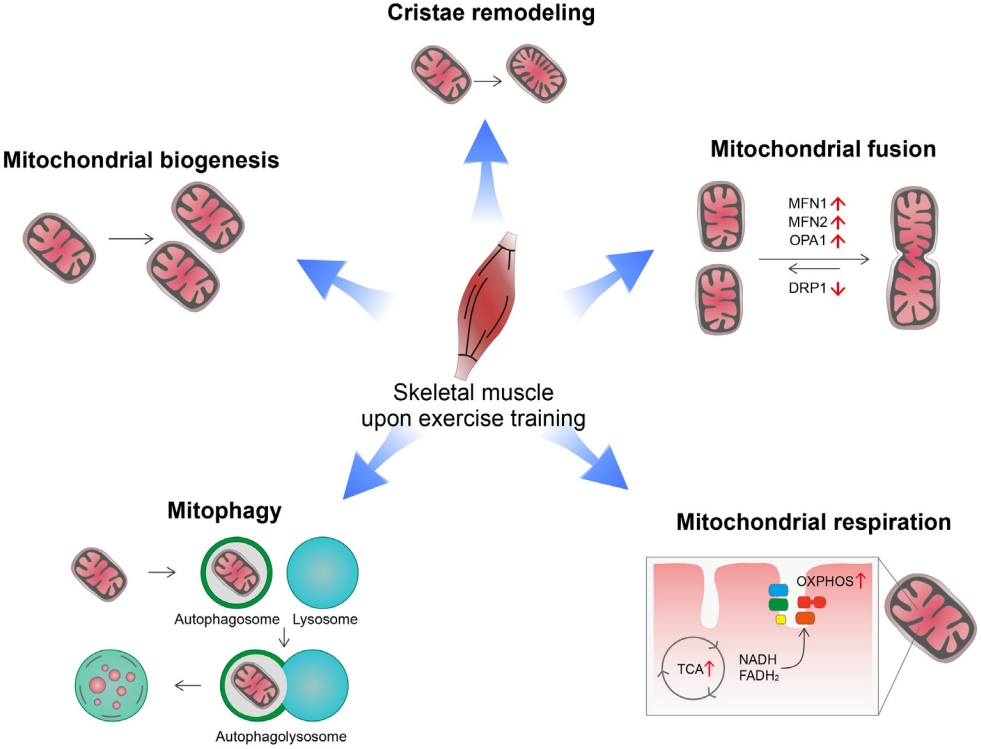
ePub - Low levels of mitochondrial stress are beneficial for organismal health and survival through a process known as mitohormesis. Mitohormetic responses occur during or after exercise and may mediate some salutary effects of exercise on metabolism. Exercise-related mitohormesis involves reactive oxygen species production, mitochondrial unfolded protein response (UPRmt), and release of mitochondria-derived peptides (MDPs). MDPs are a group of small peptides encoded by mitochondrial DNA with beneficial metabolic effects. Among MDPs, mitochondrial ORF of the 12S rRNA type-c (MOTS-c) is the most associated with exercise. MOTS-c expression levels increase in skeletal muscles, systemic circulation, and the hypothalamus upon exercise. Systemic MOTS-c administration increases exercise performance by boosting skeletal muscle stress responses and by enhancing metabolic adaptation to exercise. Exogenous MOTS-c also stimulates thermogenesis in subcutaneous white adipose tissues, thereby enhancing energy expenditure and contributing to the anti-obesity effects of exercise training. This review briefly summarizes the mitohormetic mechanisms of exercise with an emphasis on MOTS-c.
-
Citations
Citations to this article as recorded by- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
Satadeepa Kal, Sumana Mahata, Suborno Jati, Sushil K. Mahata
Peptides.2024; 172: 171147. CrossRef - Beneficial Effects of Low-Grade Mitochondrial Stress on Metabolic Diseases and Aging
Se Hee Min, Gil Myoung Kang, Jae Woo Park, Min-Seon Kim
Yonsei Medical Journal.2024; 65(2): 55. CrossRef - Roles of Myokines and Muscle-Derived Extracellular Vesicles in Musculoskeletal Deterioration under Disuse Conditions
Jie Zhang, Yunfang Gao, Jiangwei Yan
Metabolites.2024; 14(2): 88. CrossRef - Antifragility and antiinflammaging: Can they play a role for a healthy longevity?
Fabiola Olivieri, Francesco Prattichizzo, Fabrizia Lattanzio, Anna Rita Bonfigli, Liana Spazzafumo
Ageing Research Reviews.2023; 84: 101836. CrossRef - MOTS-c: A promising mitochondrial-derived peptide for therapeutic exploitation
Yuejun Zheng, Zilin Wei, Tianhui Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - MOTS-c: A potential anti-pulmonary fibrosis factor derived by mitochondria
Zewei Zhang, Dongmei Chen, Kaili Du, Yaping Huang, Xingzhe Li, Quwen Li, Xiaoting Lv
Mitochondrion.2023; 71: 76. CrossRef - Mitochondrial-Encoded Peptide MOTS-c, Diabetes, and Aging-Related Diseases
Byung Soo Kong, Changhan Lee, Young Min Cho
Diabetes & Metabolism Journal.2023; 47(3): 315. CrossRef - MOTS-c Serum Concentration Positively Correlates with Lower-Body Muscle Strength and Is Not Related to Maximal Oxygen Uptake—A Preliminary Study
Remigiusz Domin, Michał Pytka, Mikołaj Żołyński, Jan Niziński, Marcin Rucinski, Przemysław Guzik, Jacek Zieliński, Marek Ruchała
International Journal of Molecular Sciences.2023; 24(19): 14951. CrossRef - Unique Properties of Apicomplexan Mitochondria
Ian M. Lamb, Ijeoma C. Okoye, Michael W. Mather, Akhil B. Vaidya
Annual Review of Microbiology.2023; 77(1): 541. CrossRef
- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
- Cardiovascular Risk/Epidemiology
- Impact of Diabetes Control on Subclinical Atherosclerosis: Analysis from Coronary Computed Tomographic Angiography Registry
- Gyung-Min Park, Chang Hoon Lee, Seung-Whan Lee, Sung-Cheol Yun, Young-Hak Kim, Yong-Giun Kim, Ki-Bum Won, Soe Hee Ann, Shin-Jae Kim, Dong Hyun Yang, Joon-Won Kang, Tae-Hwan Lim, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Hong-Kyu Kim, Jaewon Choe, Sang-Gon Lee
- Diabetes Metab J. 2020;44(3):470-479. Published online November 22, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0073
- 8,674 View
- 69 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background There are limited data on the impact of diabetes control on the risk of subclinical coronary atherosclerosis.
Methods We analyzed 6,434 consecutive asymptomatic individuals without previous history of coronary artery disease who underwent coronary computed tomographic angiography (CCTA) (mean age, 53.7±7.6 years and 4,694 men [73.0%]). The degree and extent of subclinical coronary atherosclerosis were assessed by CCTA, and ≥50% diameter stenosis was defined as significant. A cardiac event was defined as a composite of all-cause death, myocardial infarction, unstable angina, or coronary revascularization. Study participants were categorized as normal (
n =5,319), controlled diabetes (glycosylated hemoglobin [HbA1c] <7%,n =747), or uncontrolled diabetes (HbA1c ≥7%,n =368), respectively.Results Compared with normal individuals, there were no statistically significant differences in the risk of for any atherosclerotic plaque (odds ratio [OR], 1.16; 95% confidence interval [CI], 0.98 to 1.38;
P =0.086) and significant coronary artery stenosis (OR, 1.08; 95% CI, 0.82 to 1.42;P =0.583) in controlled diabetic individuals. In contrast, uncontrolled diabetic individuals had consistently higher risks of any atherosclerotic plaque (OR, 2.16; 95% CI, 1.70 to 2.75;P <0.001) and significant coronary artery stenosis (OR, 3.34; 95% CI, 2.52 to 4.43;P <0.001) than normal individuals. During a follow-up of median 5.4 years, there was no significant difference in cardiac events between normal and controlled diabetic individuals (P =0.365). However, uncontrolled diabetes was associated with an increased risk of cardiac events compared with normal individuals (P <0.001) and controlled diabetic individuals (P =0.023).Conclusion Asymptomatic uncontrolled diabetes was associated with significant subclinical coronary atherosclerosis with subsequent high risk for cardiac events.
-
Citations
Citations to this article as recorded by- Carotid Ultrasound Abnormalities of People Living With HIV in Kunming, China: Multiple Correspondence Analysis Approach to Identify Influencing Factors
Shuishui Pan, Haiyan Fu, Zhiqiong Ai, Chongxi Li, Jinsong Bai
International Journal of STD & AIDS.2023; 34(10): 710. CrossRef - Differential Impact of Degree of Hypertension on Subclinical Coronary Atherosclerosis in Asymptomatic Subjects With and Without Diabetes Mellitus
Hyun Woo Park, Sangyong Jo, Kyung Sun Park, Hyeji Lee, Young-Jee Jeon, Sangwoo Park, Soe Hee Ann, Yong-Giun Kim, Seong Hoon Choi, Woon Jung Kwon, Young-Rak Cho, Jon Suh, Gyung-Min Park
The American Journal of Cardiology.2023; 203: 343. CrossRef - Exosomal MALAT1 Derived from High Glucose-Treated Macrophages Up-Regulates Resistin Expression via miR-150-5p Downregulation
Kou-Gi Shyu, Bao-Wei Wang, Wei-Jen Fang, Chun-Ming Pan, Chiu-Mei Lin
International Journal of Molecular Sciences.2022; 23(3): 1095. CrossRef - Comparison of Framingham risk score and pooled cohort equations for the prediction of coronary atherosclerosis in patients who meet the target LDL-C level of Korean dyslipidemia guideline
Su Bin Kim, Hae Won Jung
Medicine.2022; 101(47): e31816. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(3): 368. CrossRef - Frequency and Significance of Right Bundle Branch Block and Subclinical Coronary Atherosclerosis in Asymptomatic Individuals
Hyeji Lee, Young-Jee Jeon, Byung Ju Kang, Tae Young Lee, Eun Ji Park, Sangwoo Park, Soe Hee Ann, Yong-Giun Kim, Yongjik Lee, Seong Hoon Choi, Gyung-Min Park
The American Journal of Cardiology.2021; 158: 30. CrossRef - The association between glucose-related variables and plaque morphology in patients with ST-segment elevated myocardial infarction
Jinxin Liu, Shanjie Wang, Can Cui, Hengxuan Cai, Rong Sun, Weili Pan, Shaohong Fang, Bo Yu
Cardiovascular Diabetology.2020;[Epub] CrossRef - Choosing Antithrombotic Therapy in Patients with Coronary Heart Disease and Type 2 Diabetes Mellitus: How to Reduce the Risk of Death
N. A. Koziolova, P. G. Karavaev, A. S. Veklich
Kardiologiia.2020; 60(4): 109. CrossRef
- Carotid Ultrasound Abnormalities of People Living With HIV in Kunming, China: Multiple Correspondence Analysis Approach to Identify Influencing Factors
- Corrigendum: Figure Correction. Primary Cilia as a Signaling Platform for Control of Energy Metabolism
- Min-Seon Kim
- Diabetes Metab J. 2018;42(4):354-354. Published online August 21, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0115
- 3,009 View
- 31 Download
- Pathophysiology
- Primary Cilia as a Signaling Platform for Control of Energy Metabolism
- Do Kyeong Song, Jong Han Choi, Min-Seon Kim
- Diabetes Metab J. 2018;42(2):117-127. Published online April 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.117
- 7,931 View
- 125 Download
- 26 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Obesity has become a common healthcare problem worldwide. Cilia are tiny hair-like organelles on the cell surface that are generated and anchored by the basal body. Non-motile primary cilia have been considered to be evolutionary rudiments until a few decades, but they are now considered as important signaling organelles because many receptors, channels, and signaling molecules are highly expressed in primary cilia. A potential role of primary cilia in metabolic regulation and body weight maintenance has been suspected based on rare genetic disorders termed as ciliopathy, such as Bardet-Biedl syndrome and Alström syndrome, which manifest as obesity. Recent studies have demonstrated involvement of cilia-related cellular signaling pathways in transducing metabolic information in hypothalamic neurons and in determining cellular fate during adipose tissue development. In this review, we summarize the current knowledge about cilia and cilia-associated signaling pathways in the regulation of body metabolism.
-
Citations
Citations to this article as recorded by- MRAP2 regulates energy homeostasis by promoting primary cilia localization of MC4R
Adelaide Bernard, Irene Ojeda Naharros, Xinyu Yue, Francois Mifsud, Abbey Blake, Florence Bourgain-Guglielmetti, Jordi Ciprin, Sumei Zhang, Erin McDaid, Kellan Kim, Maxence V. Nachury, Jeremy F. Reiter, Christian Vaisse
JCI Insight.2023;[Epub] CrossRef - A high‐confidence Physcomitrium patens plasmodesmata proteome by iterative scoring and validation reveals diversification of cell wall proteins during evolution
Sven Gombos, Manuel Miras, Vicky Howe, Lin Xi, Mathieu Pottier, Neda S. Kazemein Jasemi, Moritz Schladt, J. Obinna Ejike, Ulla Neumann, Sebastian Hänsch, Franziska Kuttig, Zhaoxia Zhang, Marcel Dickmanns, Peng Xu, Thorsten Stefan, Wolfgang Baumeister, Wol
New Phytologist.2023; 238(2): 637. CrossRef - Primary cilia shape hallmarks of health and aging
Diana Filipa Silva, Cláudia Cavadas
Trends in Molecular Medicine.2023; 29(7): 567. CrossRef - Therapeutic implications of sonic hedgehog pathway in metabolic disorders: Novel target for effective treatment
Chahat Garg, Heena khan, Amarjot Kaur, Thakur Gurjeet Singh, Vivek Kumar Sharma, Sachin Kumar Singh
Pharmacological Research.2022; 179: 106194. CrossRef - Mechanisms of Weight Control by Primary Cilia
Chan Hee Lee, Gil Myoung Kang, Min-Seon Kim
Molecules and Cells.2022; 45(4): 169. CrossRef - Cilia-localized GID/CTLH ubiquitin ligase complex regulates protein homeostasis of sonic hedgehog signaling components
Friederike Hantel, Huaize Liu, Lisa Fechtner, Herbert Neuhaus, Jie Ding, Danilo Arlt, Peter Walentek, Pablo Villavicencio-Lorini, Christoph Gerhardt, Thomas Hollemann, Thorsten Pfirrmann
Journal of Cell Science.2022;[Epub] CrossRef - IFT20 governs mesenchymal stem cell fate through positively regulating TGF-β-Smad2/3-Glut1 signaling mediated glucose metabolism
Yang Li, Shuting Yang, Yang Liu, Ling Qin, Shuying Yang
Redox Biology.2022; 54: 102373. CrossRef - Primary Cilia in Pancreatic β- and α-Cells: Time to Revisit the Role of Insulin-Degrading Enzyme
Marta Pablos, Elena Casanueva-Álvarez, Carlos M. González-Casimiro, Beatriz Merino, Germán Perdomo, Irene Cózar-Castellano
Frontiers in Endocrinology.2022;[Epub] CrossRef - Palmitic acid control of ciliogenesis modulates insulin signaling in hypothalamic neurons through an autophagy-dependent mechanism
Yenniffer Ávalos, María Paz Hernández-Cáceres, Pablo Lagos, Daniela Pinto-Nuñez, Patricia Rivera, Paulina Burgos, Francisco Díaz-Castro, Michelle Joy-Immediato, Leslye Venegas-Zamora, Erik Lopez-Gallardo, Catalina Kretschmar, Ana Batista-Gonzalez, Flavia
Cell Death & Disease.2022;[Epub] CrossRef - Shedding of ciliary vesicles at a glance
Irene Ojeda Naharros, Maxence V. Nachury
Journal of Cell Science.2022;[Epub] CrossRef - Oligodendroglial primary cilium heterogeneity during development and demyelination/remyelination
Giada Delfino, Karelle Bénardais, Julien Graff, Brigitte Samama, Maria Cristina Antal, M. Said Ghandour, Nelly Boehm
Frontiers in Cellular Neuroscience.2022;[Epub] CrossRef - Proteomic and Transcriptomic Landscapes of Alström and Bardet–Biedl Syndromes
Urszula Smyczynska, Marcin Stanczak, Miljan Kuljanin, Aneta Włodarczyk, Ewelina Stoczynska-Fidelus, Joanna Taha, Bartłomiej Pawlik, Maciej Borowiec, Joseph D. Mancias, Wojciech Mlynarski, Piotr Rieske, Wojciech Fendler, Agnieszka Zmysłowska
Genes.2022; 13(12): 2370. CrossRef - A role for primary cilia in coral calcification?
Eric Tambutté, Philippe Ganot, Alexander A Venn, Sylvie Tambutté
Cell and Tissue Research.2021; 383(3): 1093. CrossRef - Myocardin-related transcription factor and serum response factor regulate cilium turnover by both transcriptional and local mechanisms
Pam Speight, Matthew Rozycki, Shruthi Venugopal, Katalin Szászi, Michael Kofler, András Kapus
iScience.2021; 24(7): 102739. CrossRef - Hypothalamic primary cilium: A hub for metabolic homeostasis
Dong Joo Yang, Jessica Hong, Ki Woo Kim
Experimental & Molecular Medicine.2021; 53(7): 1109. CrossRef - Low fluid shear stress promoted ciliogenesis via Dvl2 in hUVECs
Xin Sheng, Yan Sheng, Shuanglin Gao, Fang Fan, Junhua Wang
Histochemistry and Cell Biology.2020; 154(6): 639. CrossRef - Primary cilia mediate early life programming of adiposity through lysosomal regulation in the developing mouse hypothalamus
Chan Hee Lee, Do Kyeong Song, Chae Beom Park, Jeewon Choi, Gil Myoung Kang, Sung Hoon Shin, Ijoo Kwon, Soyoung Park, Seongjun Kim, Ji Ye Kim, Hong Dugu, Jae Woo Park, Jong Han Choi, Se Hee Min, Jong-Woo Sohn, Min-Seon Kim
Nature Communications.2020;[Epub] CrossRef - Evidences of a Direct Relationship between Cellular Fuel Supply and Ciliogenesis Regulated by Hypoxic VDAC1-ΔC
Monique Meyenberg Cunha-de Padua, Lucilla Fabbri, Maeva Dufies, Sandra Lacas-Gervais, Julie Contenti, Charles Voyton, Sofia Fazio, Marie Irondelle, Baharia Mograbi, Matthieu Rouleau, Nirvana Sadaghianloo, Amandine Rovini, Catherine Brenner, William J. Cra
Cancers.2020; 12(11): 3484. CrossRef - High-resolution characterization of centriole distal appendage morphology and dynamics by correlative STORM and electron microscopy
Mathew Bowler, Dong Kong, Shufeng Sun, Rashmi Nanjundappa, Lauren Evans, Veronica Farmer, Andrew Holland, Moe R. Mahjoub, Haixin Sui, Jadranka Loncarek
Nature Communications.2019;[Epub] CrossRef - Sonic hedgehog signaling instigates high-fat diet–induced insulin resistance by targeting PPARγ stability
Qinyu Yao, Jia Liu, Lei Xiao, Nanping Wang
Journal of Biological Chemistry.2019; 294(9): 3284. CrossRef - Cellular signalling by primary cilia in development, organ function and disease
Zeinab Anvarian, Kirk Mykytyn, Saikat Mukhopadhyay, Lotte Bang Pedersen, Søren Tvorup Christensen
Nature Reviews Nephrology.2019; 15(4): 199. CrossRef - O-GlcNAcylation Regulates Primary Ciliary Length by Promoting Microtubule Disassembly
Jie L. Tian, Hongmin Qin
iScience.2019; 12: 379. CrossRef - Interplay Between Primary Cilia and Autophagy and Its Controversial Roles in Cancer
Je Yeong Ko, Eun Ji Lee, Jong Hoon Park
Biomolecules & Therapeutics.2019; 27(4): 337. CrossRef - Neuronal and astrocytic primary cilia in the mature brain
Ashley Sterpka, Xuanmao Chen
Pharmacological Research.2018; 137: 114. CrossRef
- MRAP2 regulates energy homeostasis by promoting primary cilia localization of MC4R
- Others
- Addition of Ipragliflozin to Metformin Treatment in Korean Patients with Type 2 Diabetes Mellitus: Subgroup Analysis of a Phase 3 Trial
- Kyung-Wan Min, Bon Jeong Ku, Ji-Hyun Lee, Min-Seon Kim, Kyu-Jeung Ahn, Moon-Kyu Lee, Satoshi Kokubo, Satoshi Yoshida, Hyun-Ji Cho, Bong-Soo Cha
- Diabetes Metab J. 2017;41(2):135-145. Published online January 11, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.2.135
- 4,951 View
- 59 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This is a subgroup analysis of Korean patients from a phase 3 clinical trial investigating the efficacy and safety of ipragliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin.
Methods This multicenter, placebo-controlled, double-blind, parallel-group study was carried out between November 2011 and January 2013. Patients entered a 2-week placebo pretreatment period, followed by a 24-week treatment period with either ipragliflozin (50 mg/day) or placebo, while continuing metformin. Efficacy outcomes (glycosylated hemoglobin [HbA1c], fasting plasma glucose [FPG], and body weight) and safety outcomes (treatment-emergent adverse events [TEAEs]) were measured and compared between the two treatment groups for patients enrolled in all 18 study sites in Korea.
Results Eighty-two Korean patients received ipragliflozin (
n =43) or placebo (n =39) during the study period. Mean changes in HbA1c levels from baseline to the end of treatment were –0.97% in the ipragliflozin group and –0.31% in the placebo group, with an adjusted between-group difference of –0.60% (P <0.001). Compared to placebo, FPG and body weight also decreased significantly (bothP <0.001) from baseline after treatment in the ipragliflozin group, with between-group differences of –21.4 mg/dL and –1.53 kg, respectively. Decreased weight was the most common TEAE in the ipragliflozin group (7.0%); there were no reports of genital and urinary tract infection.Conclusion Ipragliflozin treatment in addition to metformin led to significant improvement in glycemic outcomes and reduction in body weight in Korean patients with type 2 diabetes mellitus, compared with metformin treatment alone; the safety profile was comparable in both groups.
-
Citations
Citations to this article as recorded by- Add-on therapy with dapagliflozin in routine outpatient care of type 2 diabetes patients from Turkey: a retrospective cohort study on HbA1c, body weight, and blood pressure outcomes
Derun Taner Ertugrul, Erdal Kan, Cigdem Bahadir Tura, Haci Bayram Tugtekin, Hayati Ayakta, Mehmet Celebioglu, Ceren Yılmaz, Onur Utebay, Ilhan Yetkin, Eren Gurkan, Kerem Sezer, Ramazan Gen, Suleyman Ozcaylak, Yildiz Okuturlar, Mehmet Coskun, Nilgun Govec
International Journal of Diabetes in Developing Countries.2022; 42(1): 147. CrossRef SGLT2 Inhibitors as Add-On Therapy to Metformin for People with Type 2 Diabetes: A Review of Placebo-Controlled Trials in Asian versus Non-Asian Patients
André J Scheen
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2765. CrossRef- Ipragliflozin Additively Ameliorates Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Controlled with Metformin and Pioglitazone: A 24-Week Randomized Controlled Trial
Eugene Han, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Journal of Clinical Medicine.2020; 9(1): 259. CrossRef - Safety of Ipragliflozin in Patients with Type 2 Diabetes Mellitus: Pooled Analysis of Phase II/III/IV Clinical Trials
Atsunori Kashiwagi, Marina V. Shestakova, Yuichiro Ito, Masahiro Noguchi, Wim Wilpshaar, Satoshi Yoshida, John P. H. Wilding
Diabetes Therapy.2019; 10(6): 2201. CrossRef - Mechanistic effects of SGLT2 inhibition on blood pressure in diabetes
Habib Yaribeygi, Stephen L. Atkin, Amirhossein Sahebkar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1679. CrossRef - Ipragliflozin as an add-on therapy in type 2 diabetes mellitus patients: An evidence-based pharmacoeconomics evaluation
Hongmei Wang, Gaoqiong Yao, Xi Chen, Jing Ouyang, Jiadan Yang
Diabetes Research and Clinical Practice.2019; 157: 107867. CrossRef - Characteristics of Dapagliflozin Responders: A Longitudinal, Prospective, Nationwide Dapagliflozin Surveillance Study in Korea
Eugene Han, Ari Kim, Sung Jae Lee, Je-Yon Kim, Jae Hyeon Kim, Woo Je Lee, Byung-Wan Lee
Diabetes Therapy.2018; 9(4): 1689. CrossRef - A phase 3 randomized placebo-controlled trial to assess the efficacy and safety of ipragliflozin as an add-on therapy to metformin in Russian patients with inadequately controlled type 2 diabetes mellitus
Marina V. Shestakova, John P.H. Wilding, Wim Wilpshaar, Reiner Tretter, Valeria L. Orlova, Andrey F. Verbovoy
Diabetes Research and Clinical Practice.2018; 146: 240. CrossRef - Efficacy and safety of ipragliflozin as an add‐on therapy to sitagliptin and metformin in Korean patients with inadequately controlled type 2 diabetes mellitus: A randomized controlled trial
Kyung‐Ah Han, Suk Chon, Choon Hee Chung, Soo Lim, Kwan‐Woo Lee, SeiHyun Baik, Chang Hee Jung, Dong‐Sun Kim, Kyong Soo Park, Kun‐Ho Yoon, In‐Kyu Lee, Bong‐Soo Cha, Taishi Sakatani, Sumi Park, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2018; 20(10): 2408. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Combination therapy of oral hypoglycemic agents in patients with type 2 diabetes mellitus
Min Kyong Moon, Kyu Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
The Korean Journal of Internal Medicine.2017; 32(6): 974. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon, Kyu-Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
Diabetes & Metabolism Journal.2017; 41(5): 357. CrossRef
- Add-on therapy with dapagliflozin in routine outpatient care of type 2 diabetes patients from Turkey: a retrospective cohort study on HbA1c, body weight, and blood pressure outcomes
- Clinical Features and Causes of Endogenous Hyperinsulinemic Hypoglycemia in Korea
- Chang-Yun Woo, Ji Yun Jeong, Jung Eun Jang, Jaechan Leem, Chang Hee Jung, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Jung Bok Lee, Ki-Up Lee
- Diabetes Metab J. 2015;39(2):126-131. Published online March 9, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.2.126
- 5,216 View
- 84 Download
- 22 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Endogenous hyperinsulinemic hypoglycemia (EHH) is characterized by an inappropriately high plasma insulin level, despite a low plasma glucose level. Most of the EHH cases are caused by insulinoma, whereas nesidioblastosis and insulin autoimmune syndrome (IAS) are relatively rare.
Methods To evaluate the relative frequencies of various causes of EHH in Korea, we retrospectively analyzed 84 patients who were diagnosed with EHH from 1998 to 2012 in a university hospital.
Results Among the 84 EHH patients, 74 patients (88%), five (6%), and five (6%) were diagnosed with insulinoma, nesidioblastosis or IAS, respectively. The most common clinical manifestation of EHH was neuroglycopenic symptoms. Symptom duration before diagnosis was 14.5 months (range, 1 to 120 months) for insulinoma, 1.0 months (range, 6 days to 7 months) for nesidioblastosis, and 2.0 months (range, 1 to 12 months) for IAS. One patient, who was diagnosed with nesidioblastosis in 2006, underwent distal pancreatectomy but was later determined to be positive for insulin autoantibodies. Except for one patient who was diagnosed in 2007, the remaining three patients with nesidioblastosis demonstrated severe hyperinsulinemia (157 to 2,719 µIU/mL), which suggests that these patients might have had IAS, rather than nesidioblastosis.
Conclusion The results of this study suggest that the prevalence of IAS may be higher in Korea than previously thought. Therefore, measurement of insulin autoantibody levels is warranted for EHH patients, especially in patients with very high plasma insulin levels.
-
Citations
Citations to this article as recorded by- Case report: Insulinomatosis: description of four sporadic cases and review of the literature
Delmar Muniz Lourenço, Maria Lucia Corrêa-Giannella, Sheila Aparecida Coelho Siqueira, Marcia Nery, Flavio Galvão Ribeiro, Elizangela Pereira de Souza Quedas, Manoel de Souza Rocha, Ramon Marcelino do Nascimento, Maria Adelaide Albergaria Pereira
Frontiers in Endocrinology.2024;[Epub] CrossRef - Insulin Autoimmune Syndrome: A Systematic Review
MingXu Lin, YuHua Chen, Jie Ning, Tatsuya Kin
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Diffuse, Adult-Onset Nesidioblastosis/Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS): Review of the Literature of a Rare Cause of Hyperinsulinemic Hypoglycemia
Martin Philipp Dieterle, Ayman Husari, Sophie Nicole Prozmann, Hendrik Wiethoff, Albrecht Stenzinger, Manuel Röhrich, Uwe Pfeiffer, Wolfgang Rüdiger Kießling, Helena Engel, Harald Sourij, Thorsten Steinberg, Pascal Tomakidi, Stefan Kopf, Julia Szendroedi
Biomedicines.2023; 11(6): 1732. CrossRef - An Uncommon Cause of Recurrent Presyncope, Dizziness, and Tachycardia: A Case Report of Diffuse, Adult-Onset Nesidioblastosis/Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS)
Martin Philipp Dieterle, Ayman Husari, Sophie Nicole Prozmann, Hendrik Wiethoff, Albrecht Stenzinger, Manuel Röhrich, Uwe Pfeiffer, Wolfgang Rüdiger Kießling, Helena Engel, Harald Sourij, Thorsten Steinberg, Pascal Tomakidi, Stefan Kopf, Julia Szendroedi
Biomedicines.2023; 11(6): 1741. CrossRef - An Uncommon Case of Recurrent Hypoglycemic Episodes in a Healthy Non-diabetic Male: Insulin Autoimmune Syndrome
Kanwarpal K Dhaliwal, Gaurav Bector, Saurabh Arora, Amanpreet Singh, Sanjay Kalra
Cureus.2023;[Epub] CrossRef - The After-Dinner Dip
Caren G. Solomon, Gertrud L.G. Haverkamp, Richard G. Ijzerman, Jos Kooter, Yvonne H.M. Krul-Poel
New England Journal of Medicine.2022; 386(22): 2130. CrossRef - Hirata's disease (insulin autoimmune syndrome) following envenomation by a common krait
Subramanian Senthilkumaran, Stephen W. Miller, Harry F. Williams, Ponniah Thirumalaikolundusubramanian, Sakthivel Vaiyapuri, Ketan Patel
Toxicon.2022; 219: 106923. CrossRef - Analysis of the clinical characteristics of insulin autoimmune syndrome induced by methimazole
Linli Sun, Weijin Fang, Dan Yi, Wei Sun, Chunjiang Wang
Journal of Clinical Pharmacy and Therapeutics.2021; 46(2): 470. CrossRef - Continuous glucose monitoring and Rituximab treatment in insulin autoimmune syndrome
Hiya Boro, Uttio Gupta, Charandeep Singh, Rakhi Malhotra, Rajesh Khadgawat
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(6): 102294. CrossRef Insulin Autoimmune Syndrome (Hirata Disease): A Comprehensive Review Fifty Years After Its First Description
Daniele Cappellani, Enrico Macchia, Alberto Falorni, Piero Marchetti
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 963. CrossRef- Nationwide survey of endogenous hyperinsulinemic hypoglycemia in Japan (2017–2018): Congenital hyperinsulinism, insulinoma, non‐insulinoma pancreatogenous hypoglycemia syndrome and insulin autoimmune syndrome (Hirata’s disease)
Yuki Yamada, Kana Kitayama, Maki Oyachi, Shinji Higuchi, Rie Kawakita, Yutaka Kanamori, Tohru Yorifuji
Journal of Diabetes Investigation.2020; 11(3): 554. CrossRef - Insulin Autoimmune Syndrome – A Case Series
Hiya Boro, Uttio Gupta, Charandeep Singh, Rakhi Malhotra, Rajesh Khadgawat
European Endocrinology.2020; 16(2): 168. CrossRef - Management of Insulin Autoimmune Hypoglycaemia: Single‐centre experience from Western India with systematic review of world literature
Muniraj Patel, Ravikumar Shah, Swati Ramteke‐Jadhav, Virendra Patil, Shivendra Kumar Patel, Anurag Lila, Nalini Shah, Tushar Bandgar
Clinical Endocrinology.2020; 92(5): 409. CrossRef - Is insulin intoxication still the perfect crime? Analysis and interpretation of postmortem insulin: review and perspectives in forensic toxicology
Charline Bottinelli, Nathalie Cartiser, Fabien Bévalot, Laurent Fanton, Jérôme Guitton
Critical Reviews in Toxicology.2020; 50(4): 324. CrossRef - Insulin autoimmune syndrome induced by exogenous insulin injection: a four-case series
Yimin Shen, Xiaoxiao Song, Yuezhong Ren
BMC Endocrine Disorders.2019;[Epub] CrossRef - An observational analysis of insulinoma from a single institution
S Shao, Z Zeng, S Hu
QJM: An International Journal of Medicine.2018; 111(4): 237. CrossRef - Anti-tuberculosis Treatment-Induced Insulin Autoimmune Syndrome
Jung Suk Han, Han Ju Moon, Jin Seo Kim, Hong Il Kim, Cheol Hyeon Kim, Min Joo Kim
The Ewha Medical Journal.2016; 39(4): 122. CrossRef - Spontaneous hypoglycemia: diagnostic evaluation and management
Leelavathy Kandaswamy, Rajeev Raghavan, Joseph M. Pappachan
Endocrine.2016; 53(1): 47. CrossRef - Hypoglycemia due to Insulin Autoimmune Syndrome: A rare cause not to be forgotten
Sarah Alam, Maaz Ozair, Jamal Ahmad
Journal of Clinical and Translational Endocrinology: Case Reports.2016; 2: 7. CrossRef
- Case report: Insulinomatosis: description of four sporadic cases and review of the literature
- Molecular Mechanisms of Appetite Regulation
- Ji Hee Yu, Min-Seon Kim
- Diabetes Metab J. 2012;36(6):391-398. Published online December 12, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.6.391
- 8,972 View
- 215 Download
- 80 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The prevalence of obesity has been rapidly increasing worldwide over the last several decades and has become a major health problem in developed countries. The brain, especially the hypothalamus, plays a key role in the control of food intake by sensing metabolic signals from peripheral organs and modulating feeding behaviors. To accomplish these important roles, the hypothalamus communicates with other brain areas such as the brainstem and reward-related limbic pathways. The adipocyte-derived hormone leptin and pancreatic β-cell-derived insulin inform adiposity to the hypothalamus. Gut hormones such as cholecystokinin, peptide YY, pancreatic polypeptide, glucagon-like peptide 1, and oxyntomodulin transfer satiety signals to the brain and ghrelin relays hunger signals. The endocannabinoid system and nutrients are also involved in the physiological regulation of food intake. In this article, we briefly review physiological mechanisms of appetite regulation.
-
Citations
Citations to this article as recorded by- Regulation of glycose and lipid metabolism and application based on the colloidal nutrition science properties of konjac glucomannan: A comprehensive review
Pengkui Xia, Ying Zheng, Li Sun, Wenxin Chen, Longchen Shang, Jing Li, Tao Hou, Bin Li
Carbohydrate Polymers.2024; 331: 121849. CrossRef - Weight Regain after Metabolic Surgery: Beyond the Surgical Failure
Juan Salazar, Pablo Duran, Bermary Garrido, Heliana Parra, Marlon Hernández, Clímaco Cano, Roberto Añez, Henry García-Pacheco, Gabriel Cubillos, Neidalis Vasquez, Maricarmen Chacin, Valmore Bermúdez
Journal of Clinical Medicine.2024; 13(4): 1143. CrossRef - Thylakoid supplementation and hunger and fullness perception: a systematic review and dose-response meta-analysis of randomized controlled trials
Negin Nikrad, Mehdi Ghaffari Sarghein, Mahdieh Abbasalizad Farhangi
Nutrition Reviews.2024;[Epub] CrossRef - Stomach clusterin as a gut-derived feeding regulator
Cherl NamKoong, Bohye Kim, Ji Hee Yu, Byung Soo Youn, Hanbin Kim, Evonne Kim, So Young Gil, Gil Myoung Kang, Chan Hee Lee, Young-Bum Kim, Kyeong-Han Park, Min-Seon Kim, Obin Kwon
BMB Reports.2024; 57(3): 149. CrossRef - Anorexigenic neuropeptides as anti-obesity and neuroprotective agents: exploring the neuroprotective effects of anorexigenic neuropeptides
Veronika Strnadová, Andrea Pačesová, Vilém Charvát, Zuzana Šmotková, Blanka Železná, Jaroslav Kuneš, Lenka Maletínská
Bioscience Reports.2024;[Epub] CrossRef - The non-conventional edible plant foroba (Parkia biglobosa) has anti-obesity effect, improves lipid peroxidation and reverses colon and hippocampal lesions in healthy and obese rats
Mirela Gouveia-Nhanca, Maria Luiza Rolim Bezerra, Kamila Sabino Batista, Rafael Oliveira Pinheiro, Naís Lira Soares, Maria Carolina de Paiva Sousa, Adriano Francisco Alves, Mateus Duarte Ribeiro, Alexandre Sergio Silva, Marciane Magnani, Marcos dos Santos
Journal of Functional Foods.2023; 108: 105745. CrossRef - Aberrant bone marrow-derived microglia in the hypothalamus may dysregulate appetite in diabetes
Miwako Katagi, Yuki Nakae, Junko Okano, Kazunori Fujino, Tomoki Tanaka, Itsuko Miyazawa, Natsuko Ohashi, Takahiko Nakagawa, Hideto Kojima
Biochemical and Biophysical Research Communications.2023; 682: 132. CrossRef - Proteins and peptides from vegetable food sources as therapeutic adjuvants for the type 2 diabetes mellitus
Ivan Chan-Zapata, Carlos Sandoval-Castro, Maira Rubí Segura-Campos
Critical Reviews in Food Science and Nutrition.2022; 62(10): 2673. CrossRef - Differential effects of citalopram on the intake of high fat or high carbohydrates diets in female and male rats
Amparo L. De la Fuente-Reynoso, Eliana Barrios De Tomasi, Jorge Juárez
Nutritional Neuroscience.2022; 25(7): 1477. CrossRef - Egzersizin iştah ve iştah hormonları üzerine etkisinin incelenmesi:
PubMed üzerinden yapılmış sistematik derleme
Esmanur Kaya, Şerife Vatansever
Turkish Journal of Sports Medicine.2022; 57(1): 51. CrossRef - Role of Leu72Met of GHRL and Gln223Arg of LEPR Variants on Food Intake, Subjective Appetite, and Hunger-Satiety Hormones
Tania Sanchez-Murguia, Nathaly Torres-Castillo, Lisset Magaña-de la Vega, Saraí Citlalic Rodríguez-Reyes, Wendy Campos-Pérez, Erika Martínez-López
Nutrients.2022; 14(10): 2100. CrossRef - Appetite ratings and ghrelin concentrations in young adults after administration of a balanced meal. Does sex matter?
Alessandro Leone, Ramona De Amicis, Marta Pellizzari, Simona Bertoli, Simone Ravella, Alberto Battezzati
Biology of Sex Differences.2022;[Epub] CrossRef - Interplay between fatty acid desaturase2 (FADS2) rs174583 genetic variant and dietary antioxidant capacity: cardio-metabolic risk factors in obese individuals
Mahdieh Khodarahmi, Parisa Javidzade, Mahdieh Abbasalizad Farhangi, Ahmad Hashemzehi, Houman Kahroba
BMC Endocrine Disorders.2022;[Epub] CrossRef - Appetite-regulating hormones in bipolar disorder: A systematic review and meta-analysis
Błażej Misiak, Krzysztof Kowalski, Bartłomiej Stańczykiewicz, Francesco Bartoli, Giuseppe Carrà, Jerzy Samochowiec, Agnieszka Samochowiec, Dorota Frydecka
Frontiers in Neuroendocrinology.2022; 67: 101013. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - Gut Hormones in Health and Obesity: The Upcoming Role of Short Chain Fatty Acids
Habeeb Alhabeeb, Ali AlFaiz, Emad Kutbi, Dayel AlShahrani, Abdullah Alsuhail, Saleh AlRajhi, Nemer Alotaibi, Khalid Alotaibi, Saad AlAmri, Saleh Alghamdi, Naji AlJohani
Nutrients.2021; 13(2): 481. CrossRef - Asprosin ve Glikoz Metabolizması Üzerine Etkileri
M. Gizem KESER, Nurhan ÜNÜSAN
Turkish Journal of Diabetes and Obesity.2021; 5(1): 89. CrossRef - Recent Advances in Understanding Peripheral Taste Decoding I: 2010 to 2020
Jea Hwa Jang, Obin Kwon, Seok Jun Moon, Yong Taek Jeong
Endocrinology and Metabolism.2021; 36(3): 469. CrossRef - Association of increased abdominal adiposity at birth with altered ventral caudate microstructure
Dawn X. P. Koh, Mya Thway Tint, Peter D. Gluckman, Yap Seng Chong, Fabian K. P. Yap, Anqi Qiu, Johan G. Eriksson, Marielle V. Fortier, Patricia P. Silveira, Michael J. Meaney, Ai Peng Tan
International Journal of Obesity.2021; 45(11): 2396. CrossRef - The Crosstalk Between Brain Mediators Regulating Food Intake Behavior in Birds: A Review
Behrouz Rahmani, Elham Ghashghayi, Morteza Zendehdel, Mina Khodadadi, Behnam Hamidi
International Journal of Peptide Research and Therapeutics.2021; 27(4): 2349. CrossRef - Oral Semaglutide, the First Ingestible Glucagon-Like Peptide-1 Receptor Agonist: Could It Be a Magic Bullet for Type 2 Diabetes?
Hwi Seung Kim, Chang Hee Jung
International Journal of Molecular Sciences.2021; 22(18): 9936. CrossRef - Potential Role of Hypothalamic and Plasma Ghrelin in the Feeding Behavior of Obese Type 2 Diabetic Rats with Intraventricular Glucagon-Like Peptide-1 Receptor Agonist Intervention
Ke Lu, Xiaoyan Chen, Xuelian Deng, Juan Long, Jianhua Yan
Obesity Facts.2021; 14(1): 10. CrossRef - Managing obesity through natural polyphenols: A review
Manisha Singh, Thilini Thrimawithana, Ravi Shukla, Benu Adhikari
Future Foods.2020; 1-2: 100002. CrossRef - Neurochemical regulators of food behavior for pharmacological treatment of obesity: current status and future prospects
Gayane Sargis Vardanyan, Hasmik Samvel Harutyunyan, Michail Iosif Aghajanov, Ruben Sargis Vardanyan
Future Medicinal Chemistry.2020; 12(20): 1865. CrossRef - Modulation of feeding behavior and metabolism by dynorphin
Aishwarya Ghule, Ildiko Rácz, Andras Bilkei-Gorzo, Este Leidmaa, Meike Sieburg, Andreas Zimmer
Scientific Reports.2020;[Epub] CrossRef - Possible role of peptide YY (PYY) in the pathophysiology of irritable bowel syndrome (IBS)
Magdy El-Salhy, Jan Gunnar Hatlebakk, Trygve Hausken
Neuropeptides.2020; 79: 101973. CrossRef - Prolactin-releasing peptide increases food intake and affects hypothalamic physiology in Japanese quail (Coturnix japonica)
B.R. McConn, T. Tachibana, E.R. Gilbert, M.A. Cline
Domestic Animal Endocrinology.2020; 72: 106464. CrossRef - Obesity induced by Borna disease virus in rats: key roles of hypothalamic fast-acting neurotransmitters and inflammatory infiltrates
Georg Gosztonyi, Hanns Ludwig, Liv Bode, Moujahed Kao, Manfred Sell, Peter Petrusz, Béla Halász
Brain Structure and Function.2020; 225(5): 1459. CrossRef - D‐methionine improves cisplatin‐induced anorexia and dyspepsia syndrome by attenuating intestinal tryptophan hydroxylase 1 activity and increasing plasma leptin concentration
Yi‐Sin Wong, Meei‐Yn Lin, Pei‐Fen Liu, Jiunn‐Liang Ko, Guan‐Ting Huang, Dom‐Gene Tu, Chu‐Chyn Ou
Neurogastroenterology & Motility.2020;[Epub] CrossRef - Effects of oral, smoked, and vaporized cannabis on endocrine pathways related to appetite and metabolism: a randomized, double-blind, placebo-controlled, human laboratory study
Mehdi Farokhnia, Gray R. McDiarmid, Matthew N. Newmeyer, Vikas Munjal, Osama A. Abulseoud, Marilyn A. Huestis, Lorenzo Leggio
Translational Psychiatry.2020;[Epub] CrossRef - Role of Paraventricular Nucleus in Regulation of Feeding Behaviour and the Design of Intranuclear Neuronal Pathway Communications
Shiba Yousefvand, Farshid Hamidi
International Journal of Peptide Research and Therapeutics.2020; 26(3): 1231. CrossRef - Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study
Jia-Yi Dong, Satoyo Ikehara, Takashi Kimura, Meishan Cui, Yoko Kawanishi, Tadashi Kimura, Kimiko Ueda, Hiroyasu Iso
Nutrients.2020; 12(5): 1296. CrossRef - Effects of a high-fat-diet supplemented with probiotics and ω3-fatty acids on appetite regulatory neuropeptides and neurotransmitters in a pig model
D. Valent, L. Arroyo, E. Fàbrega, M. Font-i-Furnols, M. Rodríguez-Palmero, J.A. Moreno-Muñoz, J. Tibau, A. Bassols
Beneficial Microbes.2020; 11(4): 347. CrossRef - Electro-Acupuncture Alleviates Cisplatin-Induced Anorexia in Rats by Modulating Ghrelin and Monoamine Neurotransmitters
Ji Yun Baek, Tuy An Trinh, Wonsang Huh, Ji Hoon Song, Hyun Young Kim, Juhee Lim, Jinhee Kim, Hyun Jin Choi, Tae-Hun Kim, Ki Sung Kang
Biomolecules.2019; 9(10): 624. CrossRef - Interleukin-6 Expression by Hypothalamic Microglia in Multiple Inflammatory Contexts: A Systematic Review
Vanessa C. D. Bobbo, Carlos P. Jara, Natália F. Mendes, Joseane Morari, Lício A. Velloso, Eliana P. Araújo
BioMed Research International.2019; 2019: 1. CrossRef - Abnormalities in Glucose Metabolism, Appetite-Related Peptide Release, and Pro-inflammatory Cytokines Play a Central Role in Appetite Disorders in Peritoneal Dialysis
Lorena Avila-Carrasco, Mario A. Pavone, Elena González, Álvaro Aguilera-Baca, Rafael Selgas, Gloria del Peso, Secundino Cigarran, Manuel López-Cabrera, Abelardo Aguilera
Frontiers in Physiology.2019;[Epub] CrossRef - Branched chain amino acids stimulate gut satiety hormone cholecystokinin secretion through activation of the umami taste receptor T1R1/T1R3 using an in vitro porcine jejunum model
Min Tian, Jinghui Heng, Hanqing Song, Yufeng Zhang, Fang Chen, Wutai Guan, Shihai Zhang
Food & Function.2019; 10(6): 3356. CrossRef - Multi-Omic Biological Age Estimation and Its Correlation With Wellness and Disease Phenotypes: A Longitudinal Study of 3,558 Individuals
John C Earls, Noa Rappaport, Laura Heath, Tomasz Wilmanski, Andrew T Magis, Nicholas J Schork, Gilbert S Omenn, Jennifer Lovejoy, Leroy Hood, Nathan D Price, David Le Couteur
The Journals of Gerontology: Series A.2019; 74(Supplement): S52. CrossRef - The impact of sugar consumption on stress driven, emotional and addictive behaviors
Angela Jacques, Nicholas Chaaya, Kate Beecher, Syed Aoun Ali, Arnauld Belmer, Selena Bartlett
Neuroscience & Biobehavioral Reviews.2019; 103: 178. CrossRef - Leptin Signaling in the Control of Metabolism and Appetite: Lessons from Animal Models
Alberto A. Barrios-Correa, José A. Estrada, Irazú Contreras
Journal of Molecular Neuroscience.2018; 66(3): 390. CrossRef - Role of paraventricular hypothalamic dopaminergic D1 receptors in food intake regulation of food-deprived rats
Zahra. Mirmohammadsadeghi, Masoud. Shareghi Brojeni, Abbas. Haghparast, Afsaneh. Eliassi
European Journal of Pharmacology.2018; 818: 43. CrossRef - Integrating Thyroid Hormone Signaling in Hypothalamic Control of Metabolism: Crosstalk Between Nuclear Receptors
Soumaya Kouidhi, Marie-Stéphanie Clerget-Froidevaux
International Journal of Molecular Sciences.2018; 19(7): 2017. CrossRef - Review article: Role of satiety hormones in anorexia induction by Trichothecene mycotoxins
Chloé Terciolo, Marc Maresca, Philippe Pinton, Isabelle P. Oswald
Food and Chemical Toxicology.2018; 121: 701. CrossRef - Obezite ve Ghrelin/Leptin İlişkisi
Aliye Sağkan Öztürk, Abdullah ARPACI
Mustafa Kemal Üniversitesi Tıp Dergisi.2018; 9(35): 136. CrossRef - Overexpression of Wild-Type Human Alpha-Synuclein Causes Metabolism Abnormalities in Thy1-aSYN Transgenic Mice
Elodie Cuvelier, Mathieu Méquinion, Coline Leghay, William Sibran, Aliçia Stievenard, Alessia Sarchione, Marie-Amandine Bonte, Christel Vanbesien-Mailliot, Odile Viltart, Kevin Saitoski, Emilie Caron, Alexandra Labarthe, Thomas Comptdaer, Pierre Semaille,
Frontiers in Molecular Neuroscience.2018;[Epub] CrossRef - Aetiology of eating behaviours: A possible mechanism to understand obesity development in early childhood
Nikki Boswell, Rebecca Byrne, Peter S.W. Davies
Neuroscience & Biobehavioral Reviews.2018; 95: 438. CrossRef - Clinical Phenotype of Depression Affects Interleukin-6 Synthesis
Łukasz Zadka, Piotr Dzięgiel, Michał Kulus, Marcin Olajossy
Journal of Interferon & Cytokine Research.2017; 37(6): 231. CrossRef - Altered Adipogenesis in Zebrafish Larvae Following High Fat Diet and Chemical Exposure Is Visualised by Stimulated Raman Scattering Microscopy
Marjo den Broeder, Miriam Moester, Jorke Kamstra, Peter Cenijn, Valentina Davidoiu, Leonie Kamminga, Freek Ariese, Johannes de Boer, Juliette Legler
International Journal of Molecular Sciences.2017; 18(4): 894. CrossRef - SIFamide Translates Hunger Signals into Appetitive and Feeding Behavior in Drosophila
Carlotta Martelli, Ulrike Pech, Simon Kobbenbring, Dennis Pauls, Britta Bahl, Mirjam Vanessa Sommer, Atefeh Pooryasin, Jonas Barth, Carmina Warth Perez Arias, Chrystalleni Vassiliou, Abud Jose Farca Luna, Haiko Poppinga, Florian Gerhard Richter, Christian
Cell Reports.2017; 20(2): 464. CrossRef - Effect of Mulberry Extract on the Lipid Profile and Liver Function in Mice Fed a High Fat Diet
Kyung-Soon Choi, Yong-Hwan Kim, Kyung-Ok Shin
The Korean Journal of Food And Nutrition.2016; 29(3): 411. CrossRef - Helicobacter pylori Infection in Children: Nutritional Status and Associations with Serum Leptin, Ghrelin, and IGF‐1 Levels
Gulin Erdemir, Tanju Basarir Ozkan, Taner Ozgur, Derya Altay, Sinan Cavun, Guher Goral
Helicobacter.2016; 21(4): 317. CrossRef - Dietary Capsaicin Protects Cardiometabolic Organs from Dysfunction
Fang Sun, Shiqiang Xiong, Zhiming Zhu
Nutrients.2016; 8(5): 174. CrossRef - Effects of Short-Term Exenatide Treatment on Regional Fat Distribution, Glycated Hemoglobin Levels, and Aortic Pulse Wave Velocity of Obese Type 2 Diabetes Mellitus Patients
Ju-Young Hong, Keun-Young Park, Byung-Joon Kim, Won-Min Hwang, Dong-Ho Kim, Dong-Mee Lim
Endocrinology and Metabolism.2016; 31(1): 80. CrossRef - The role of the neuropeptide Y (NPY) family in the pathophysiology of inflammatory bowel disease (IBD)
Magdy El-Salhy, Trygve Hausken
Neuropeptides.2016; 55: 137. CrossRef - Proactive and Progressive Approaches in Managing Obesity
Robert H. Eckel, Harold E. Bays, Samuel Klein, Deborah Bade Horn
Postgraduate Medicine.2016; 128(sup1): 21. CrossRef - The role of food intake regulating peptides in cardiovascular regulation
B. Mikulášková, L. Maletínská, J. Zicha, J. Kuneš
Molecular and Cellular Endocrinology.2016; 436: 78. CrossRef - Altered gut and adipose tissue hormones in overweight and obese individuals: cause or consequence?
M E J Lean, D Malkova
International Journal of Obesity.2016; 40(4): 622. CrossRef - Expression of NUCB2/nesfatin-1 in the taste buds of rats
Xun Cao, Xiao Zhou, Yang Cao, Xiao-Min Liu, Li-Hong Zhou
Endocrine Journal.2016; 63(1): 37. CrossRef - Brain Regulation of Energy Metabolism
Eun Roh, Min-Seon Kim
Endocrinology and Metabolism.2016; 31(4): 519. CrossRef - Stopped-Flow Studies of the Reduction of the Copper Centers Suggest a Bifurcated Electron Transfer Pathway in Peptidylglycine Monooxygenase
Shefali Chauhan, Parisa Hosseinzadeh, Yi Lu, Ninian J. Blackburn
Biochemistry.2016; 55(13): 2008. CrossRef - Potential role of bioactive compounds of Phaseolus vulgaris L. on lipid-lowering mechanisms
Aurea K. Ramírez-Jiménez, Rosalía Reynoso-Camacho, M. Elizabeth Tejero, Fabiola León-Galván, Guadalupe Loarca-Piña
Food Research International.2015; 76: 92. CrossRef - Recent developments in the pathophysiology of irritable bowel syndrome
Magdy El-Salhy
World Journal of Gastroenterology.2015; 21(25): 7621. CrossRef - Lifestyle Changes Followed by Bariatric Surgery Lower Inflammatory Markers and the Cardiovascular Risk Factors C3 and C4
Torunn Kristin Nestvold, Erik Waage Nielsen, Judith Krey Ludviksen, Hilde Fure, Anne Landsem, Knut Tore Lappegård
Metabolic Syndrome and Related Disorders.2015; 13(1): 29. CrossRef - Diet in irritable bowel syndrome
Magdy El-Salhy, Doris Gundersen
Nutrition Journal.2015;[Epub] CrossRef - 3p22.1p21.31 microdeletion identifies CCK as Asperger syndrome candidate gene and shows the way for therapeutic strategies in chromosome imbalances
Ivan Y. Iourov, Svetlana G. Vorsanova, Victoria Y. Voinova, Yuri B. Yurov
Molecular Cytogenetics.2015;[Epub] CrossRef - The effect of slow spaced eating on hunger and satiety in overweight and obese patients with type 2 diabetes mellitus
Theodoros Angelopoulos, Alexander Kokkinos, Christos Liaskos, Nicholas Tentolouris, Kleopatra Alexiadou, Alexander Dimitri Miras, Iordanis Mourouzis, Despoina Perrea, Constantinos Pantos, Nicholas Katsilambros, Stephen R Bloom, Carel Wynard le Roux
BMJ Open Diabetes Research & Care.2014; 2(1): e000013. CrossRef - Bisphenol A is related to circulating levels of adiponectin, leptin and ghrelin, but not to fat mass or fat distribution in humans
Monika Rönn, Lars Lind, Jan Örberg, Joel Kullberg, Stefan Söderberg, Anders Larsson, Lars Johansson, Håkan Ahlström, P. Monica Lind
Chemosphere.2014; 112: 42. CrossRef - The modulatory role of alpha-melanocyte stimulating hormone administered spinally in the regulation of blood glucose level in d-glucose-fed and restraint stress mouse models
Yun-Beom Sim, Soo-Hyun Park, Sung-Su Kim, Su-Min Lim, Jun-Sub Jung, Hong-Won Suh
Neuropeptides.2014; 48(4): 207. CrossRef - The forgotten members of the glucagon family
Dominique Bataille, Stéphane Dalle
Diabetes Research and Clinical Practice.2014; 106(1): 1. CrossRef - Incretin mimetics as pharmacologic tools to elucidate and as a new drug strategy to treat traumatic brain injury
Nigel H. Greig, David Tweedie, Lital Rachmany, Yazhou Li, Vardit Rubovitch, Shaul Schreiber, Yung-Hsiao Chiang, Barry J. Hoffer, Jonathan Miller, Debomoy K. Lahiri, Kumar Sambamurti, Robert E. Becker, Chaim G. Pick
Alzheimer's & Dementia.2014;[Epub] CrossRef - Fatty acid analysis and regulatory effects of citron (Citrus junosSieb. ex TANAKA) seed oil on nitric oxide production, lipid accumulation, and leptin secretion
Tae Woo Kim, Kyoung Kon Kim, Yun Hwan Kang, Dae Jung Kim, Myeon Choe
Journal of Nutrition and Health.2014; 47(4): 221. CrossRef - Analysis of Pine Nut Oil Composition and Its Effects on Obesity
Kyoung Kon Kim, Yun Hwan Kang, Dae Jung Kim, Tae Woo Kim, Myeon Choe
Korean Journal of Food Science and Technology.2014; 46(5): 630. CrossRef - Anti-obesity effects of KR-66195, a synthetic DPP-IV inhibitor, in diet-induced obese mice and obese-diabetic ob/ob mice
Eun Young Lee, Yeon Wook Kim, Hyunhee Oh, Cheol Soo Choi, Jin Hee Ahn, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Metabolism.2014; 63(6): 793. CrossRef - Position and Length of Fatty Acids Strongly Affect Receptor Selectivity Pattern of Human Pancreatic Polypeptide Analogues
Veronika Mäde, Kathrin Bellmann‐Sickert, Anette Kaiser, Jens Meiler, Annette G. Beck‐Sickinger
ChemMedChem.2014; 9(11): 2463. CrossRef - Regulation of food intake after surgery and the gut brain axis
Nilanjana Tewari, Sherif Awad, Dileep N. Lobo
Current Opinion in Clinical Nutrition and Metabolic Care.2013; 16(5): 569. CrossRef - Effect of ambient temperature during acute aerobic exercise on short-term appetite, energy intake, and plasma acylated ghrelin in recreationally active males
Lucy K. Wasse, James A. King, David J. Stensel, Caroline Sunderland
Applied Physiology, Nutrition, and Metabolism.2013; 38(8): 905. CrossRef - Peripheral Pathways in the Food-Intake Control towards the Adipose-Intestinal Missing Link
Hugo Mendieta Zerón, Ma. Victoria Domínguez García, María del Socorro Camarillo Romero, Miriam V. Flores-Merino
International Journal of Endocrinology.2013; 2013: 1. CrossRef - Alteration of sweet taste in high-fat diet induced obese rats after 4 weeks treatment with exenatide
Xiao-juan Zhang, Yu-qing Wang, Yang Long, Lei Wang, Yun Li, Fa-bao Gao, Hao-ming Tian
Peptides.2013; 47: 115. CrossRef - Decrease of Obesity by Allantoin via Imidazoline I1-Receptor Activation in High Fat Diet-Fed Mice
Hsien-Hui Chung, Kung Shing Lee, Juei-Tang Cheng
Evidence-Based Complementary and Alternative Medicine.2013; 2013: 1. CrossRef - Hunger Hormone Profile Monitoring after Gastroplication in an Adolescent
Valeria Calcaterra, Gloria Pelizzo, Ghassan Nakib, Daniela Larizza, Maria Luisa Fonte, Mara De Amici, Hellas Cena
Hormone Research in Paediatrics.2013; 80(3): 213. CrossRef
- Regulation of glycose and lipid metabolism and application based on the colloidal nutrition science properties of konjac glucomannan: A comprehensive review
- Various Oscillation Patterns of Serum Fibroblast Growth Factor 21 Concentrations in Healthy Volunteers
- Sang Ah Lee, Eunheiu Jeong, Eun Hee Kim, Mi-Seon Shin, Jenie Yoonoo Hwang, Eun Hee Koh, Woo Je Lee, Joong-Yeol Park, Min-Seon Kim
- Diabetes Metab J. 2012;36(1):29-36. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.29
- 3,653 View
- 32 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Fibroblast growth factor 21 (FGF21) was originally identified as a paroxysm proliferator activated receptor-α target gene product and is a hormone involved in metabolic regulation. The purpose of this study was to investigate the diurnal variation of serum FGF21 concentration in obese and non-obese healthy volunteers.
Methods Blood samples were collected from five non-obese (body mass index [BMI] ≤23 kg/m2) and five obese (BMI ≥25 kg/m2) healthy young men every 30 to 60 minutes over 24 hours. Serum FGF21 concentrations were determined by radioimmunoassay. Anthropometric parameters, glucose, free fatty acid, insulin, leptin, and cortisol concentrations were also measured.
Results The serum FGF21 concentrations displayed various individual oscillation patterns. The oscillation frequency ranged between 6 and 12 times per day. The average duration of oscillation was 2.52 hours (range, 1.9 to 3.0 hours). The peaks and troughs of FGF21 oscillation showed no circadian rhythm. However, the oscillation frequency had a diurnal variation and was lower during the light-off period than during the light-on period (2.4 vs. 7.3 times,
P <0.001). There was no difference in the total frequency or duration of oscillations between non-obese and obese subjects, but obese individuals had increased numbers of larger oscillations (amplitude ≥0.19 ng/mL).Conclusion Various oscillation patterns in serum FGF21 concentration were observed, and reduced oscillation frequencies were seen during sleep. The oscillation patterns of serum FGF21 concentration suggest that FGF21 may be secreted into systemic circulation in a pulsatile manner. Obesity appeared to affect the amplitude of oscillations of serum FGF21.
-
Citations
Citations to this article as recorded by- Circadian Regulation of Endocrine Fibroblast Growth Factors on Systemic Energy Metabolism
Zhenning Yang, Helmut Zarbl, Grace L. Guo
Molecular Pharmacology.2024; 105(3): 179. CrossRef - Acute sleep loss alters circulating fibroblast growth factor 21 levels in humans: A randomised crossover trial
Luiz Eduardo Mateus Brandão, Daniel Espes, Jakub Orzechowski Westholm, Teemu Martikainen, Nestori Westerlund, Lauri Lampola, Alexandru Popa, Heike Vogel, Annette Schürmann, Suzanne L. Dickson, Christian Benedict, Jonathan Cedernaes
Journal of Sleep Research.2022;[Epub] CrossRef - Metabolic Stress Index Including Mitochondrial Biomarker for Noninvasive Diagnosis of Hepatic Steatosis
Jae Seung Chang, Jhii-Hyun Ahn, Seong Hee Kang, Sang-Baek Koh, Jang-Young Kim, Soon Koo Baik, Ji Hye Huh, Samuel S. Lee, Moon Young Kim, Kyu-Sang Park
Frontiers in Endocrinology.2022;[Epub] CrossRef - Single-Arm 8-Week Ad Libitum Self-Prepared Paleo Diet Reduces Cardiometabolic Disease Risk Factors in Overweight Adults
Melissa M. Markofski, Kristofer Jennings, Chad Dolan, Natalie A. Davies, Emily C. LaVoy, Edward J. Ryan, Andres E. Carrillo
American Journal of Lifestyle Medicine.2021; 15(6): 690. CrossRef - Diurnal rhythm in clinical chemistry: An underrated source of variation
Mohamed Abou El Hassan, Edgard Delvin, Manal O. Elnenaei, Barry Hoffman
Critical Reviews in Clinical Laboratory Sciences.2018; 55(8): 516. CrossRef - Integrated stress response stimulates FGF21 expression: Systemic enhancer of longevity
Antero Salminen, Kai Kaarniranta, Anu Kauppinen
Cellular Signalling.2017; 40: 10. CrossRef - Therapeutic potential of the endocrine fibroblast growth factors FGF19, FGF21 and FGF23
Chiara Degirolamo, Carlo Sabbà, Antonio Moschetta
Nature Reviews Drug Discovery.2016; 15(1): 51. CrossRef - Response of fibroblast growth factor 21 to meal intake and insulin infusion in patients on maintenance haemodialysis
Mark Reinhard, Jan Frystyk, Bente Jespersen, Else Randers, Bo Martin Bibby, Per Ivarsen
Clinical Endocrinology.2015; 83(2): 187. CrossRef - Possible role of fibroblast growth factor 21 on atherosclerosis via amelioration of endoplasmic reticulum stress-mediated apoptosis in apoE−/− mice
Xi Wu, Yong-Fen Qi, Jin-Rui Chang, Wei-Wei Lu, Jin-Sheng Zhang, Shao-Ping Wang, Shu-Juan Cheng, Ming Zhang, Qian Fan, Yuan Lv, Hui Zhu, Man-Kun Xin, Yun Lv, Jing-Hua Liu
Heart and Vessels.2015; 30(5): 657. CrossRef - Circulating Fibroblast Growth Factors as Metabolic Regulators—A Critical Appraisal
Bo Angelin, Tobias E. Larsson, Mats Rudling
Cell Metabolism.2012; 16(6): 693. CrossRef - Metabolic actions of fibroblast growth factor 21
Daniel Cuevas-Ramos, Carlos A. Aguilar-Salinas, Francisco J. Gómez-Pérez
Current Opinion in Pediatrics.2012; 24(4): 523. CrossRef - Fibroblast Growth Factor 21: A Novel Metabolic Regulator
Ji A Seo, Nan Hee Kim
Diabetes & Metabolism Journal.2012; 36(1): 26. CrossRef - MECHANISMS IN ENDOCRINOLOGY: Biological role, clinical significance, and therapeutic possibilities of the recently discovered metabolic hormone fibroblastic growth factor 21
Pedro Iglesias, Rafael Selgas, Sara Romero, Juan J Díez
European Journal of Endocrinology.2012; 167(3): 301. CrossRef
- Circadian Regulation of Endocrine Fibroblast Growth Factors on Systemic Energy Metabolism
- The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital
- Ji Hee Yu, Jenie Yoonoo Hwang, Mi-Seon Shin, Chang Hee Jung, Eun Hee Kim, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Diabetes Metab J. 2011;35(5):543-550. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.543
- 4,266 View
- 49 Download
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Peripheral arterial disease (PAD) is a common manifestation of systemic atherosclerosis and is associated with significant morbidity and mortality. Diabetes is known to increase the risk of PAD two- to four-fold. The prevalence of PAD in Korean diabetic patients has not been established. In this study, we investigated the prevalence of PAD in Korean patients with type 2 diabetes attending a large university hospital and analyzed the factors associated with PAD.
Methods A total of 2,002 patients with type 2 diabetes who underwent ankle-brachial index (ABI) measurement in an outpatient clinic were enrolled. PAD was defined as an ABI ≤0.9. Clinical characteristics of 64 patients with PAD were compared with those of 192 age- and sex-matched control patients without PAD.
Results Of the 2,002 type 2 diabetic patients, 64 (3.2%) were diagnosed as having PAD. PAD was associated with higher prevalences of retinopathy, nephropathy, neuropathy, cerebrovascular and coronary artery disease. Patients with PAD had higher systolic blood pressure and serum triglyceride level and reported higher pack-years of smoking. Multivariate analysis showed that the presence of micro- and macrovascular complications and high systolic blood pressure are factors independently associated with PAD.
Conclusion The prevalence of PAD in diabetic patients was 3.2%, suggesting that the prevalence in Korean diabetic patients is lower than that of patients in Western countries.
-
Citations
Citations to this article as recorded by- Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
Nibedita Priyadarsini, Devineni Likhitha, Madumathy Ramachandran, Kishore Kumar Behera
Canadian Journal of Diabetes.2023;[Epub] CrossRef - The Predictability of Cystatin C for Peripheral Arterial Disease in Chinese Population with Type 2 Diabetes Mellitus
Luna Liu, Hai Wang, Jing Ning, Junming Han, Chunxiao Yu, Qingbo Guan, Hiroshi Okamoto
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Atherectomy in Peripheral Artery Disease: Current and Future
Yohan Kwon, Jinoo Kim, Je-Hwan Won, Seong Ho Kim, Jeong-Eun Kim, Sung-Joon Park
Journal of the Korean Society of Radiology.2021; 82(3): 551. CrossRef - Peripheral arterial disease and its correlates in patients with type 2 diabetes mellitus in a teaching hospital in northern Nigeria: a cross-sectional study
Orighomisan Freda Agboghoroma, Fatai Momodu Akemokwe, Fabian H. Puepet
BMC Cardiovascular Disorders.2020;[Epub] CrossRef - The significance of ankle-brachial index in determining peripheral artery disease in patients with type 2 diabetes mellitus over 40 years of age and the relationship of peripheral artery disease with chronic complications of diabetes
Tuğçe Nur YİĞENOĞLU, Medine KEBAPÇI, Hülya ÖZEN
Journal of Health Sciences and Medicine.2020; 3(2): 115. CrossRef - Correlation of systemic arterial stiffness with changes in retinal and choroidal microvasculature in type 2 diabetes
Mirinae Kim, Rae-Young Kim, Joo-Young Kim, Young-Hoon Park
Scientific Reports.2019;[Epub] CrossRef - Abnormally Low or High Ankle-Brachial Index Is Associated With the Development of Diabetic Retinopathy in Type 2 Diabetes Mellitus
Mei-Yueh Lee, Pi-Jung Hsiao, Jiun-Chi Huang, Wei-Hao Hsu, Szu-Chia Chen, Jer-Ming Chang, Shyi–Jang Shin
Scientific Reports.2018;[Epub] CrossRef - Peripheral Arterial Disease in Type 2 Diabetes Is Associated with an Increase in Fibrinogen Levels
Qin-Fen Chen, Dan Cao, Ting-Ting Ye, Hui-Hui Deng, Hong Zhu
International Journal of Endocrinology.2018; 2018: 1. CrossRef - Association between peripheral arterial disease and diabetic foot ulcers in patients with diabetes mellitus type 2
M.Á. Tresierra-Ayala, A. García Rojas
Medicina Universitaria.2017; 19(76): 123. CrossRef - Factors associated with lower extremity atherosclerotic disease in Chinese patients with type 2 diabetes mellitus
Qingge Gao, Binbin He, Chaoyu Zhu, Yuanyuan Xiao, Li Wei, Weiping Jia
Medicine.2016; 95(51): e5230. CrossRef - Significant interarm blood pressure difference predicts cardiovascular risk in hypertensive patients
Su-A Kim, Jang Young Kim, Jeong Bae Park
Medicine.2016; 95(24): e3888. CrossRef - 7th Asian PAD Workshop
Annals of Vascular Diseases.2016; 9(2): 135. CrossRef - 6th Asian PAD Workshop
Annals of Vascular Diseases.2015; 8(2): 135. CrossRef - Abnormally Low or High Ankle-Brachial Index Is Associated with Proliferative Diabetic Retinopathy in Type 2 Diabetic Mellitus Patients
Szu-Chia Chen, Pi-Jung Hsiao, Jiun-Chi Huang, Kun-Der Lin, Wei-Hao Hsu, Yu-Li Lee, Mei-Yueh Lee, Jer-Ming Chang, Shyi–Jang Shin, Xiao-Feng Yang
PLOS ONE.2015; 10(7): e0134718. CrossRef - Identification of peripheral arterial disease in diabetic patients and its association with quality of life, physical activity and body composition
Ana Tereza do Nascimento Sales, Guilherme Augusto de Freitas Fregonezi, Ana Gabriela Câmara Batista Silva, Cibele Teresinha Dias Ribeiro, Mario Emílio Teixeira Dourado-Junior, André Gustavo Pires Sousa, Fernando Augusto Lavezzo Dias
Jornal Vascular Brasileiro.2015; 14(1): 46. CrossRef - Chronic venous ulceration of leg associated with peripheral arterial disease: an underappreciated entity in developing country
Falguni Nag, Abhishek De, Avijit Hazra, Gobinda Chatterjee, Arghyaprasun Ghosh, Trupti V Surana
International Wound Journal.2014; 11(5): 546. CrossRef - Photoplethysmography and Continuous-Wave Doppler Ultrasound as a Complementary Test to Ankle–Brachial Index in Detection of Stenotic Peripheral Arterial Disease
Du Hyun Ro, Hyuk Ju Moon, Ji Hyeung Kim, Kyoung Min Lee, Sung Ju Kim, Dong Yeon Lee
Angiology.2013; 64(4): 314. CrossRef - Ankle brachial index as a predictor of subclinical atherosclerosis in the elderly
Ilker Tasci, Samet Verim, Hasan Kutsi Kabul, Aydogan Aydogdu
International Journal of Cardiology.2012; 160(2): 147. CrossRef - Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction
Jinkwon Kim, Dong Hyun Lee, Myoung-Jin Cha, Tae-Jin Song, Ji Hye Park, Hye Sun Lee, Chung Mo Nam, Hyo Suk Nam, Young Dae Kim, Ji Hoe Heo
Atherosclerosis.2012; 224(1): 113. CrossRef - Letter: The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital (Diabetes Metab J 2011;35:543-50)
Won Jun Kim, Cheol-Young Park
Diabetes & Metabolism Journal.2011; 35(6): 637. CrossRef
- Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
- Homocysteine as a Risk Factor for Development of Microalbuminuria in Type 2 Diabetes
- Eun-Hee Cho, Eun Hee Kim, Won Gu Kim, Eun Hui Jeong, Eun Hee Koh, Woo-Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Korean Diabetes J. 2010;34(3):200-206. Published online June 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.3.200
- 3,567 View
- 26 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Kidney function is critical in homocysteine clearance, and plasma homocysteine level is frequently increased in patients with renal failure. On the other hand, recent studies in animals have shown that hyperhomocysteinemia induces renal injury. In this study, we determined whether hyperhomocysteinemia can be a risk factor for the development of microalbuminuria in patients with type 2 diabetes.
Methods A nested case-control study. Of 887 patients with type 2 diabetes who did not have microalbuminuria at baseline, 76 developed microalbuminuria during follow-up (mean, 36.0 ± 11.7 months; range, 18 to 76 months). The control group consisted of 152 age- and sex-matched subjects who did not develop microalbuminuria. Baseline plasma homocysteine concentrations were measured in stored samples.
Results Baseline plasma homocysteine concentrations and mean HbA1C levels during follow-up were significantly higher in patients who developed microalbuminuria than in those who remained normoalbuminuric. Multivariate logistic regression analysis showed that baseline plasma homocysteine level and mean HbA1C were independent predictors of microalbuminuria in type 2 diabetes.
Conclusion Hyperhomocysteinemia was associated with increased risk of microalbuminuria in patients with type 2 diabetes supporting the concept that hyperhomocysteinemia has an etiologic role in the pathogenesis of diabetic nephropathy.
-
Citations
Citations to this article as recorded by- Homocysteine and diabetes: Role in macrovascular and microvascular complications
Emir Muzurović, Ivana Kraljević, Mirsala Solak, Siniša Dragnić, Dimitri P. Mikhailidis
Journal of Diabetes and its Complications.2021; 35(3): 107834. CrossRef - Associations of Homocysteine with B Vitamins and Zinc in Serum Levels of Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study
Sadako MATSUI, Chika HIRAISHI, Ryo SATO, Takai KOJIMA, Kiyotaka ANDO, Kei FUJIMOTO, Hiroshi YOSHIDA
Journal of Nutritional Science and Vitaminology.2021; 67(6): 417. CrossRef - A risk scoring system for the decreased glomerular filtration rate in Chinese general population
Yan Gu, Min Chen, Bei Zhu, Xiaohua Pei, Zhenzhu Yong, Xiaona Li, Qun Zhang, Weihong Zhao
Journal of Clinical Laboratory Analysis.2020;[Epub] CrossRef - Relationship between plasma total homocysteine and the severity of renal function in Chinese patients with type 2 diabetes mellitus aged ≥75 years
Ning Ma, Ning Xu, Dong Yin, Weiwei Liu, Mengping Wu, Xingbo Cheng
Medicine.2020; 99(27): e20737. CrossRef - Correlation between serum homocysteine level and ulcerative colitis: A meta-analysis
Yifang Zhong, Feng Yan, Weixia Jie, Ying Zhou, Fang Fang
Pteridines.2019; 30(1): 114. CrossRef - The role of molecular genetic alterations in genes involved in folate and homocysteine metabolism in multifactorial diseases pathogenesis
A. M. Burdennyy, V. I. Loginov, T. M. Zavarykina, E. A. Braga, A. A. Kubatiev
Russian Journal of Genetics.2017; 53(5): 528. CrossRef - МОЛЕКУЛЯРНО-ГЕНЕТИЧЕСКИЕ НАРУШЕНИЯ ГЕНОВ ФОЛАТНОГО И ГОМОЦИСТЕИНОВОГО ОБМЕНА В ПАТОГЕНЕЗЕ РЯДА МНОГОФАКТОРНЫХ ЗАБОЛЕВАНИЙ, "Генетика"
А. М. Бурдённый, В.И. Логинов, Т.М. Заварыкина, Э.А. Брага, А.А. Кубатиев
Генетика.2017; (5): 526. CrossRef - Association Between Plasma Homocysteine and Microalbuminuria in Untreated Patients with Essential Hypertension: a Case-Control Study
Ze-min Kuang, Ying Wang, Shu-jun Feng, Long Jiang, Wen-li Cheng
Kidney and Blood Pressure Research.2017; 42(6): 1303. CrossRef - NMDA Receptors as Potential Therapeutic Targets in Diabetic Nephropathy: Increased Renal NMDA Receptor Subunit Expression in Akita Mice and Reduced Nephropathy Following Sustained Treatment With Memantine or MK-801
Hila Roshanravan, Eun Young Kim, Stuart E. Dryer
Diabetes.2016; 65(10): 3139. CrossRef - Association between homocysteine status and the risk of nephropathy in type 2 diabetes mellitus
Song Mao, Wei Xiang, Songming Huang, Aihua Zhang
Clinica Chimica Acta.2014; 431: 206. CrossRef - Prevalence and Determinants of Diabetic Nephropathy in Korea: Korea National Health and Nutrition Examination Survey
Jae Hee Ahn, Ji Hee Yu, Seung-Hyun Ko, Hyuk-Sang Kwon, Dae Jung Kim, Jae Hyeon Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Soo Lim, Sung Hee Choi, Kyungdo Han, Bong-Yun Cha, Nan Hee Kim
Diabetes & Metabolism Journal.2014; 38(2): 109. CrossRef - Plasma Homocysteine level and its clinical correlation with type 2 diabetes mellitus and its complications
Satyendra Kumar Sonkar, Gyanendra Kumar Sonkar, Deepika Soni, Dheeraj Soni, Kauser Usman
International Journal of Diabetes in Developing Countries.2014; 34(1): 3. CrossRef - Genetic Predisposition for Development of Nephropathy in Type 2 Diabetes Mellitus
Ravindra Kumar, Raj Kumar Sharma, Sarita Agarwal
Biochemical Genetics.2013; 51(11-12): 865. CrossRef - Is C677T Polymorphism in Methylenetetrahydrofolate Reductase Gene a Risk Factor for Diabetic Nephropathy or Diabetes Mellitus in a Chinese Population?
Wen-peng Cui, Bing Du, Ye Jia, Wen-hua Zhou, Sheng-mao Liu, Ying-chun Cui, Fu-zhe Ma, Ping Luo, Li-ning Miao
Archives of Medical Research.2012; 43(1): 42. CrossRef - The role of coagulation and inflammation in the development of diabetic nephropathy in patients withdiabetes mellitus type 2
Yulia Valer'evna Khasanova, Alsu Asatovna Nelaeva, Anna Borisovna Galkina, Irina Vasil'evna Medvedeva
Diabetes mellitus.2012; 15(1): 31. CrossRef
- Homocysteine and diabetes: Role in macrovascular and microvascular complications
- Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients
- Eun Hee Kim, Ji Hee Yu, Sang Ah Lee, Eui Young Kim, Won Gu Kim, Seung Hun Lee, Eun Hee Cho, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Korean Diabetes J. 2010;34(2):95-100. Published online April 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.2.95
- 4,414 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Serum cystatin C level is a more sensitive marker of renal dysfunction than serum creatinine level. Serum cystatin C level was recently reported to predict the development of cardiovascular disease. This study was performed to evaluate whether the cystatin C level is associated with coronary artery disease (CAD), independent of diabetic nephropathy.
Methods We conducted a case-control study to assess the relationship between serum cystatin C level and coronary artery disease in diabetic patients. Among 460 diabetic patients, 38 diabetic patients had CAD. The control group consisted of 38 diabetic patients who were matched to cases by age, sex, and presence/absence of diabetic nephropathy. Serum cystatin C level was measured in stored samples.
Results Serum cystatin C level was significantly higher in patients with diabetic nephropathy, both in CAD and non-CAD patients. However, serum cystatin C level did not differ between CAD and non-CAD patients, regardless of diabetic nephropathy.
Conclusion Serum cystatin C level is a marker of renal dysfunction, but not coronary artery disease, in diabetic patients.
-
Citations
Citations to this article as recorded by- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome
Gordana Dragović, Danica Srdić, Khawla Al Musalhi, Ivan Soldatović, Jovana Kušić, Djordje Jevtović, Devaki Nair
Basic & Clinical Pharmacology & Toxicology.2018; 122(4): 396. CrossRef - The association between serum cystatin C and carotid intima–media thickness in metabolic syndrome patients with normal estimated glomerular filtration rate
Rong Huang, Jingli Gu, Qin Cao, Jiahua Ma, Weiwei Gu, Zhuping Fan
Clinica Chimica Acta.2015; 448: 170. CrossRef - Association of plasma cystatin C levels with angiographically documented coronary artery disease in patients of Indian origin
Aditya Batra, Aditya Kapoor, R.K. Sharma, Nitin Agrawal, Archana Sinha, Sudeep Kumar, Naveen Garg, Satyendra Tewari, Pravin K. Goel
Journal of Cardiology.2012; 59(2): 182. CrossRef - Cystatin C and asymptomatic coronary artery disease in patients with metabolic syndrome and normal glomerular filtration rate
Xie Qing, Wang Furong, Liu Yunxia, Zhang Jian, Wang Xuping, Gao Ling
Cardiovascular Diabetology.2012;[Epub] CrossRef - Response: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Eun Hee Kim, Ki-Up Lee
Korean Diabetes Journal.2010; 34(3): 209. CrossRef - Serum Cystatin C as a Biomarker for Predicting Coronary Artery Disease in Diabetes
Jee-Young Oh
Korean Diabetes Journal.2010; 34(2): 84. CrossRef - Letter: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Kyu-Chang Won
Korean Diabetes Journal.2010; 34(3): 207. CrossRef
- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome

 KDA
KDA
 First
First Prev
Prev





